Stem cell 'major discovery' claimed
This is big.
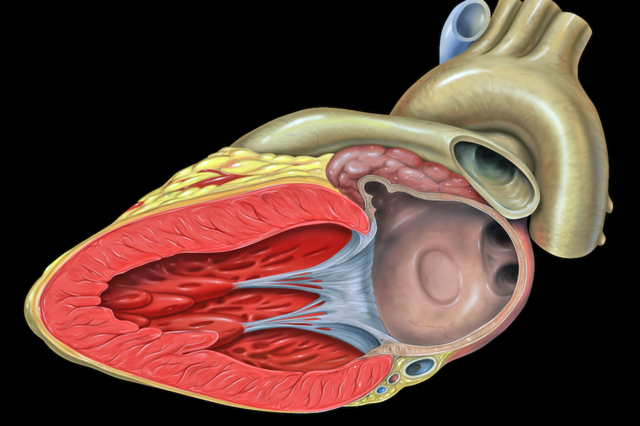
Scientists have found a way to create embryonic stem cells without using an embryo or without introducing genetic material. The discovery could revolutionize medicine by giving doctors a way to repair diseased and damaged tissue — think heart disease, blindness, skin burns — with organs and tissue grown from the patient’s own cells.
Stem cell researchers are heralding a "major scientific discovery", with the potential to start a new age of personalised medicine.
Scientists in Japan showed stem cells can now be made quickly just by dipping blood cells into acid.
Stem cells can transform into any tissue and are already being trialled for healing the eye, heart and brain.
The latest development, published in the journal Nature, could make the technology cheaper, faster and safer.
The human body is built of cells with a specific role - nerve cells, liver cells, muscle cells - and that role is fixed.
However, stem cells can become any other type of cell, and they have become a major field of research in medicine for their potential to regenerate the body.
Embryos are one, ethically charged, source of stem cells. Nobel prize winning research also showed that skin cells could be "genetically reprogrammed" to become stem cells (termed induced pluripotent stem cells).
Now a study shows that shocking blood cells with acid could also trigger the transformation into stem cells - this time termed STAP (stimulus-triggered acquisition of pluripotency) cells.
Dr Haruko Obokata, from the Riken Centre for Developmental Biology in Japan, said she was "really surprised" that cells could respond to their environment in this way.
She added: "It's exciting to think about the new possibilities these findings offer us, not only in regenerative medicine, but cancer as well."
The breakthrough was achieved in mouse blood cells, but research is now taking place to achieve the same results with human blood.
Chris Mason, professor of regenerative medicine at University College London, said if it also works in humans then "the age of personalised medicine would have finally arrived."
He told the BBC: "I thought - 'my God that's a game changer!' It's a very exciting, but surprise, finding.
"It looks a bit too good to be true, but the number of experts who have reviewed and checked this, I'm sure that it is.
"If this works in people as well as it does in mice, it looks faster, cheaper and possibly safer than other cell reprogramming technologies - personalised reprogrammed cell therapies may now be viable."
For age-related macular degeneration, which causes sight loss, it takes 10 months to go from a patient's skin sample to a therapy that could be injected into their eye -and at huge cost.
Prof Mason said weeks could be knocked off that time which would save money, as would cheaper components.
'Revolutionary'
The finding has been described as "remarkable" by the Medical Research Council's Prof Robin Lovell-Badge and as "a major scientific discovery" by Dr Dusko Ilic, a reader in stem cell science at Kings College London.
Dr Ilic added: "The approach is indeed revolutionary.
"It will make a fundamental change in how scientists perceive the interplay of environment and genome."
But he added: "It does not bring stem cell-based therapy closer. We will need to use the same precautions for the cells generated in this way as for the cells isolated from embryos or reprogrammed with a standard method."
And Prof Lovell-Badge said: "It is going to be a while before the nature of these cells are understood, and whether they might prove to be useful for developing therapies, but the really intriguing thing to discover will be the mechanism underlying how a low pH shock triggers reprogramming - and why it does not happen when we eat lemon or vinegar or drink cola?"
Read More on: 1. http://news.discovery.com/tech/biotechnology/groundbreaking-embryonic-stem-cells-made-with-acid-140129.html