Damaged or diseased organs may someday be healed with an injection of blood vessel cells, eliminating the need for donated organs and transplants, according to scientists at Weill Cornell Medical College....ya this research news is not latest as it appear in beginning of oct but i thought it's really amazing if someone has not notice can make out from my blog.....
It appears that providing endothelial cells to an organ helps that organ repair itself. Rather than 3D printed organs or iPS cells being used to grow a new organ from scratch, organ renewal may be as simple as culturing some endothelial cells and injecting them directly into the damaged/diseased organ! We may be closer to organ regeneration that we thought...
In studies appearing in recent issues ofStem Cell Journal and Developmental Cell, the researchers show that endothelial cells -- the cells that make up the structure of blood vessels -- are powerful biological machines that drive regeneration in organ tissues by releasing beneficial, organ-specific molecules.
They discovered this by decoding the entirety of active genes in endothelial cells, revealing hundreds of known genes that had never been associated with these cells. The researchers also found that organs dictate the structure and function of their own blood vessels, including the repair molecules they secrete.
Together, the studies show that endothelial cells and the organs they are transplanted into work together to repair damage and restore function, says the study's lead investigator, Shahin Rafii, M.D., a professor of genetic medicine and co-director of the medical college's Ansary Stem Cell Institute and Tri-SCI Stem Center. When an organ is injured, its blood vessels may not be able to repair the damage on their own because they may themselves be harmed or inflamed, says Dr. Rafii, who is also an investigator at the Howard Hughes Medical Institute.
"Our work suggests that that an infusion of engineered endothelial cells could engraft into injured tissue and acquire the capacity to repair the organ," he says. "These studies -- along with the first molecular atlas of organ-specific blood vessel cells reported in the Developmental Cell paper-- will open up a whole new chapter in translational vascular medicine and will have major therapeutic application.
"Scientists had thought blood vessels in each organ are the same, that they exist to deliver oxygen and nutrients. But they are very different," and each organ is endowed with blood vessels with unique shape and function and delegated with the difficult task of complying with the metabolic demands of that organ, Dr. Rafii adds.
Creating an endothelial cell genetic 'atlas'
In the Developmental Cell study, the research team examined nine different tissues at homeostasis -- a steady, healthy state -- as well as liver and bone marrow recovering from a traumatic injury.
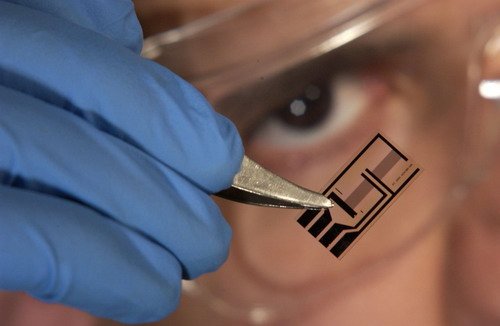
The scientists developed technology that helped them obtain "a pure population of endothelial cells in a very rapid time frame," says the study's lead author, Dr. Daniel Nolan, a senior scientist in Dr. Rafii's laboratory during this study who became an employee of Angiocrine Bioscience after it was completed. AB is housed at Weill Cornell Medical College and founded on various technologies based on Dr. Rafii's work.
From these cells, they were able to take a snapshot of all the genes that are being expressed in the various populations of endothelial cells known as vascular beds.
They found that endothelial cells possess tissue-specific genes that code for unique growth factors, adhesion molecules, and factors regulating metabolism. "We knew that these gene products were critical to the health of a particular tissue, but before our study it was not appreciated that these factors originate in the endothelial cells," Dr. Nolan says.
"We also found that the healing, or regeneration of tissue, in the liver and in the bone marrow were unexpectedly different -- including the repair molecules, known as angiocrine growth factors, that were expressed by the endothelial cells," says Dr. Olivier Elemento, who performed the complex computational calculations for the studies.
Blood vessels differ among various organs because the endothelial cells have to constantly adapt to the metabolic, biomechanical, inflammatory and immunological needs of that particular organ, says Dr. Michael Ginsberg, a senior postdoctoral associate in Dr. Rafii's laboratory during this study. Ginsberg also became an employee of Angiocrine Bioscience after the study ended. "And we have now found how endothelial cells have learned to behave differently in each organ and adjust to the needs of those organs," he says.
These findings raise the question as to how endothelial cells have the capacity to adapt to the biological demands of each organ. Is it possible to design "immature" endothelial cells that could allow scientists to identify the means by which the microenvironmental cues educate them to become more specialized endothelial cells?
"Versatile endothelial cells" for organ therapy
To address this issue, the scientists postulated that endothelial cells derived from embryonic stem cells could behave as resilient endothelial cells, being able to be taught how to act like an organ-specific blood vessel. Indeed, in the Stem Cell Journalstudy, the team generated endothelial cells from mouse embryonic stem cells that were functional, transplantable and responsive to microenvironmental signals.
These embryonic-derived endothelial cells "are versatile, so they can be transplanted into different tissues, become educated by the tissue, and acquire the characteristics of the native endothelial cells," says the study's senior author, Dr. Sina Rabbany, an adjunct associate professor of genetic medicine and bioengineering in medicine at Weill Cornell Medical College.
Dr. Rabbany says researchers can propagate these cells in large numbers in the laboratory. "We now know what it takes to keep these cells healthy, stable and viable for transplantation," he says.
In fact, in the Developmental Cell study, the researchers transplanted these generic endothelial cells generated by Dr. Rabbany's team into the liver of a mouse and found that it became indistinguishable from native endothelial cells. This also occurred when cells were grafted into kidneys. "These naive endothelial cells acquire the phenotype -- the molecular profile and signature -- of the native pre-existing endothelial cells due to the unique microenvironment in the organ," Dr. Ginsberg says.
"These transplanted endothelial cells are being educated by the unique biophysical mincroenvironment organ in which they are placed. They morph into endothelial cells that belong in the organ, and that can repair it," he adds. "If you have a heart injury and you need to reform some of your cardiomyocytes, the endothelial cells that are around the heart secrete factors that are specific for helping a heart repair itself," Dr. Rabbany says.
However, to translate these studies to the clinical setting the scientists have to generate endothelial cells that have similar immune constitution -"immunocompatible" with the recipient patient. "Endothelial cells could be derived from human embryonic pluripotent stem cells as well as by somatic cell nuclear transfer (SCNT)," says Dr. Zev Rosenwaks, director and physician-in-chief of the Ronald O. Perelman and Claudia Cohen Center for Reproductive Medicine and director of the Stem Cell Derivation Laboratory of Weill Cornell Medical College and a co-author on the studies. "In the SCNT approach, the nucleus of a somatic cell is introduced into the human egg resulting in the generation of embryonic stem cells that would generate endothelial cells that are a genetic match of the patient," says Dr. Daylon James, assistant professor of reproductive biology at Weill Cornell, who was instrumental in designing protocols to generate endothelial cells from human embryonic stem cells.
"Alternatively, to overcome the bioethical issues associated with human embryos or eggs and potential predisposition of the embryonic stem cells to produce cancer cells, one can take cells discarded after a diagnostic prenatal amniocentesis and turn them into endothelial cells capable of repairing and regenerating blood vessels. Freezing and stockpiling such cells will allow transplantation of these cells to a genetically diverse population of patients," adds Dr. Rosenwaks, referring to work published last October in the journal Cell. Ginsberg is an inventor on this technology, which Angiocrine has licensed.
Additional preclinical investigation is required before study of endothelial cell transplantation in humans is possible, but the therapeutic potential of endothelial cell transplantation is endless, Dr. Rafii says. "They could also be used as Trojan horses to block tumor growth, they could be altered to carry toxic chemicals. They could become biological cruise missiles, directed to do many things inside diseased organs," he says. "Our work has just begun."
via science daily